Keratosis pilaris is one of the most common yet misunderstood skin conditions. Often described as “chicken skin,” it causes rough, tiny bumps on the arms, thighs, cheeks, or buttocks.
While harmless, it can significantly affect confidence and skin texture — particularly in adults who value smooth, even-toned skin.
At Emirates Dermatology & Cosmetology Center (EDCC) in Abu Dhabi, keratosis pilaris is treated using a structured, consultant-led dermatological protocol focused on correcting abnormal keratinization safely and effectively.
Table of Contents
- What Is Keratosis Pilaris?
- What Causes Keratosis Pilaris?
- Symptoms and Common Areas Affected
- Why Keratosis Pilaris Is Common in Middle Eastern Skin
- Why Home Remedies and Scrubs Fail
- Consultant Dermatologist Treatment Approach at EDCC
- Specially Compounded Prescription Therapy
- Long-Term Maintenance Strategy
- Keratosis Pilaris vs. Similar Conditions
- Frequently Asked Questions
- When to See a Dermatologist in Abu Dhabi
What Is Keratosis Pilaris?
Keratosis pilaris is a chronic follicular keratinization disorder.
It occurs when keratin — the protective protein in skin — accumulates inside hair follicles instead of shedding normally.
This leads to:
- Micro-plug formation
- Rough texture
- Small bumps
- Occasional redness
- Secondary pigmentation
Medically, this is referred to as follicular hyperkeratosis.
The central issue is not dryness — it is abnormal keratin retention.
What Causes Keratosis Pilaris?
Keratosis pilaris has:
- Genetic predisposition
- Association with dry skin
- Links to atopic tendency
- Worsening in dry climates
In Abu Dhabi, environmental factors such as:
- Air conditioning
- Heat
- Low humidity indoors
can aggravate barrier dysfunction and make the condition more noticeable.
Symptoms and Common Areas Affected
Most commonly affected areas include:
- Upper arms
- Thighs
- Buttocks
- Cheeks (especially in children)
Typical symptoms:
- Sandpaper-like texture
- Flesh-colored or red bumps
- Dry patches
- Mild itching
- Post-inflammatory hyperpigmentation
In darker skin types, pigmentation can become more concerning than the bumps themselves.
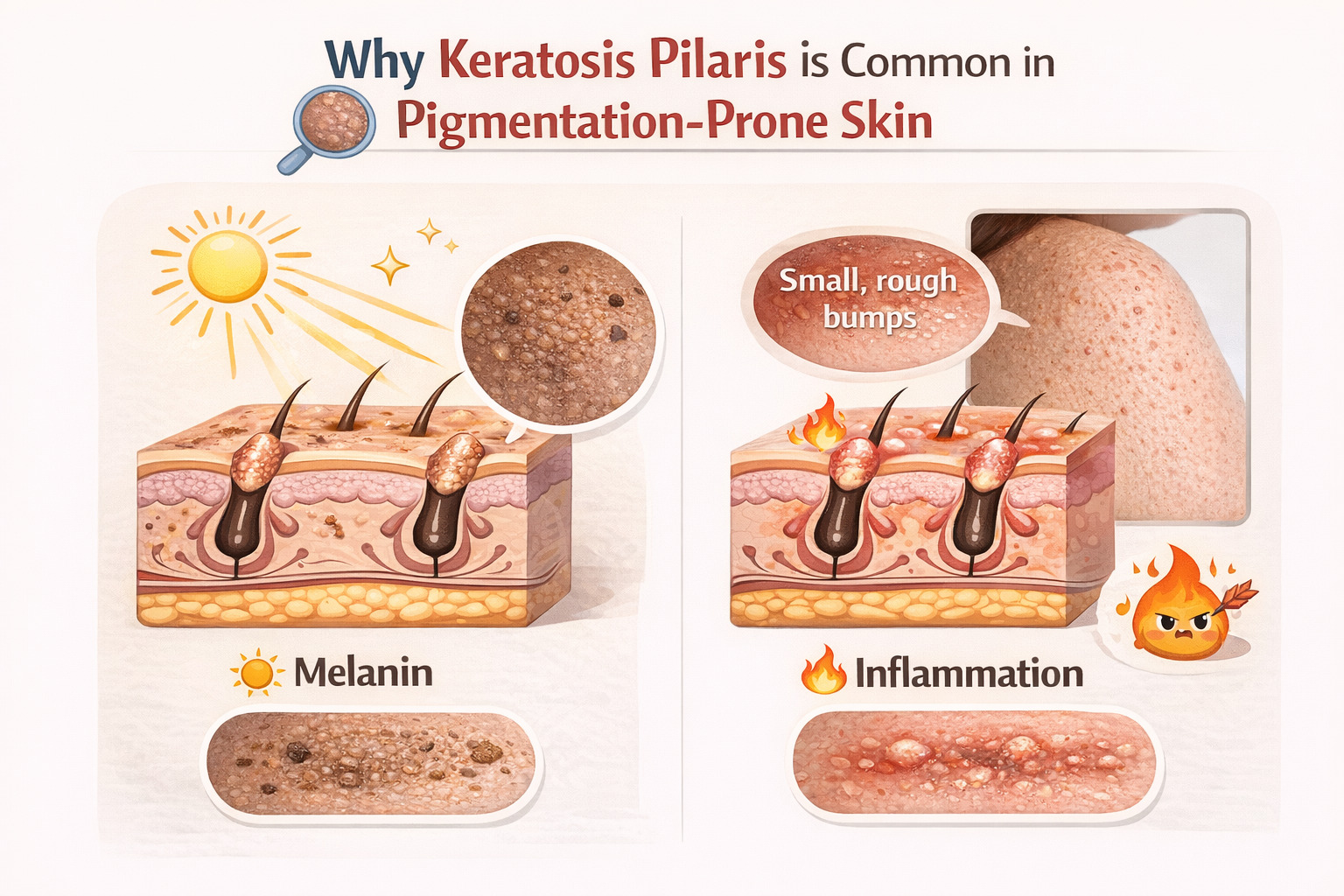
Why Keratosis Pilaris Is Common in Pigmentation-Prone Skin
Middle Eastern skin types (Fitzpatrick III–V) are more prone to:
- Post-inflammatory hyperpigmentation
- Persistent discoloration after irritation
- Barrier disruption from over-exfoliation
Aggressive scrubbing often worsens pigmentation more than the original condition.
This is why medical supervision is critical.
Why Home Remedies and Scrubs Fail
Many patients attempt:
- Physical scrubs
- Loofahs
- Random acid layering
- Over-the-counter retinoids
These may flatten bumps temporarily but:
- Do not dissolve deep keratin plugs
- Disrupt barrier integrity
- Trigger irritation
- Increase pigmentation risk
Keratosis pilaris requires controlled
keratolysis, not mechanical abrasion.
Consultant Dermatologist Treatment Approach at EDCC
At Emirates Dermatology & Cosmetology Center, treatment is individualized.
Step 1 – Detailed Dermatological Assessment
Evaluation includes:
- Severity grading
- Inflammation level
- Pigmentation risk
- Barrier resilience
- Differential diagnosis exclusion
This ensures accurate treatment selection.
Step 2 – Controlled Medical Exfoliation
Dermatologist-supervised keratolytic resurfacing:
- Dissolves retained keratin
- Reduces follicular obstruction
- Improves texture
- Enhances absorption of prescription therapy
Depth and formulation are carefully selected to protect pigmentation-prone skin.
Specially Compounded Prescription Therapy (Core of Treatment)
The foundation of long-term control is custom-compounded dermatological therapy.
Unlike standard commercial creams, compounded formulations allow:
- Precise adjustment of urea concentration
- Controlled alpha-hydroxy acid levels
- Beta-hydroxy acid inclusion
- Topical retinoid modulation
- Anti-inflammatory agents
- Pigment-modulating components (when needed)
Why Compounded Therapy Outperforms OTC Products
- Optimized concentrations
- Synergistic combinations
- Reduced irritation
- Barrier preservation
- Safer for darker skin types
This is medical keratin regulation — not cosmetic smoothing.
Long-Term Maintenance Strategy
Keratosis pilaris is chronic but manageable.
Maintenance includes:
- Scheduled keratolytic cycles
- Barrier repair support
- Pigmentation prevention
- Seasonal adjustments
Consistency under supervision ensures long-term improvement.
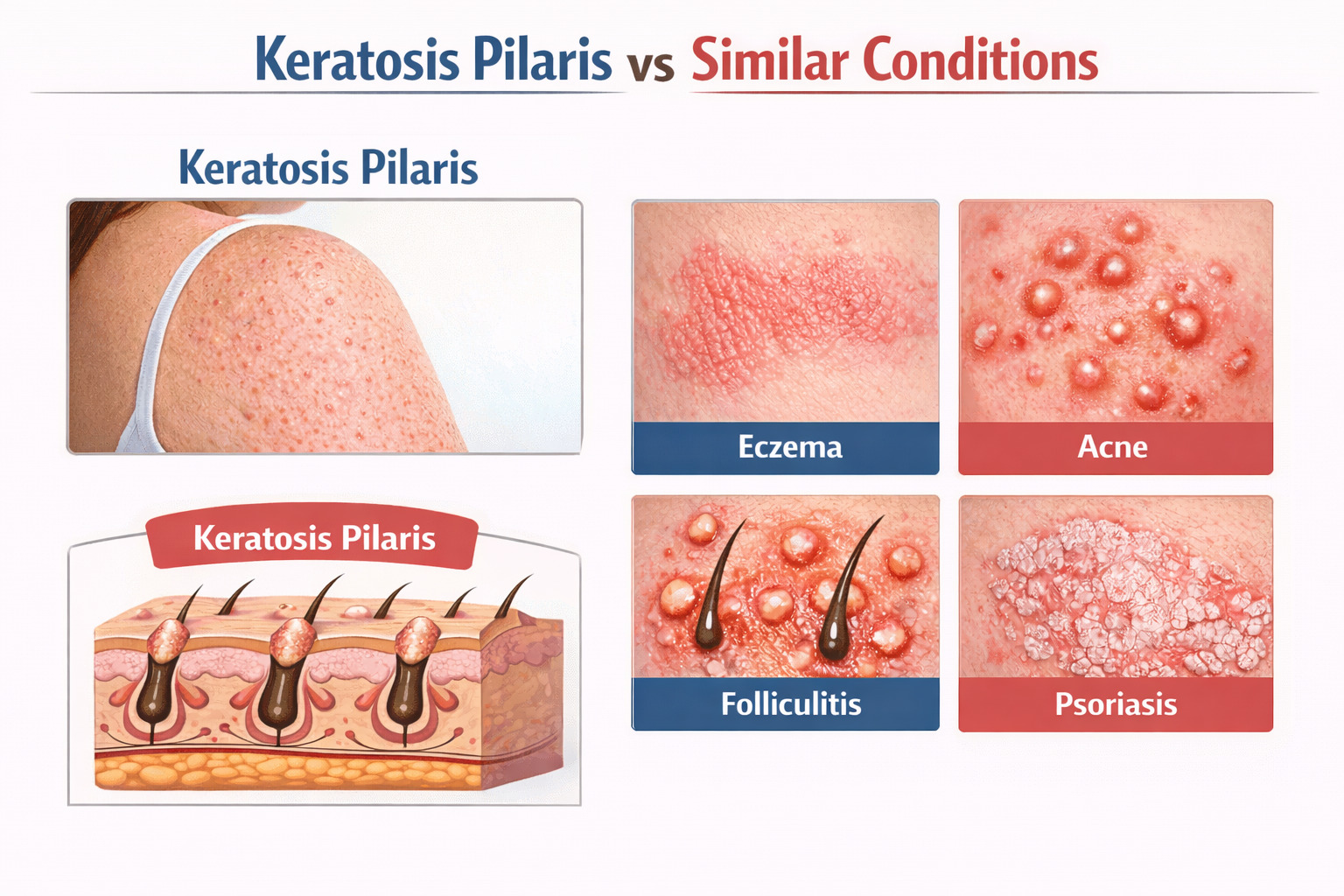
Keratosis Pilaris vs. Similar Conditions
Proper diagnosis is essential.
Conditions that may resemble keratosis pilaris:
- Acne
- Folliculitis
- Atopic xerosis
- Lichen spinulosus
Misdiagnosis leads to ineffective treatment.
A consultant-level assessment ensures correct management.
Frequently Asked Questions
Is keratosis pilaris permanent?
It is chronic but controllable.
Does moisturizing cure it?
No. Moisturizers support the barrier but do not remove keratin plugs.
Are compounded treatments safe?
Yes, when prescribed by a Consultant Dermatologist and tailored to skin type.
How long until improvement?
Texture improvement typically begins within weeks under structured therapy.
When to See a Dermatologist in Abu Dhabi
You should seek specialist evaluation if:
- Bumps persist for years
- Pigmentation develops
- Over-the-counter products fail
- Skin becomes irritated from scrubbing
Early intervention prevents long-term discoloration.
Why Choose EDCC for Keratosis Pilaris Treatment in Abu Dhabi
- Consultant Dermatologist-led care
- Evidence-based pathology-driven approach
- Customized compounded prescriptions
- Expertise in pigmentation-prone skin
- Long-term management strategy
At Emirates Dermatology & Cosmetology Center, treatment focuses on correction — not temporary cosmetic smoothing.
Book a Specialist Consultation
If rough, bumpy skin affects your confidence, structured dermatological treatment can restore smooth texture safely.
Schedule a consultation for keratosis pilaris treatment in Abu Dhabi at EDCC.